Osteoarthritis Disease Progression and How to Slow It
- BCI Health Team

- 3 days ago
- 7 min read
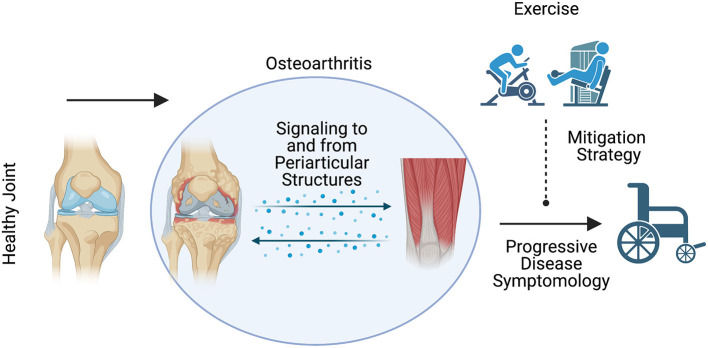
When you hear the phrase 'osteoarthritis progression,' it's easy to imagine a rapid, inevitable decline. But for most people, the reality is a slow journey. Understanding osteoarthritis disease progression—the basic osteoarthritis pathobehind joint changes—is the first step toward managing your symptoms effectively.
Think of a healthy joint as a perfectly engineered hinge. The ends of your bones are capped with a smooth, slippery cushion called cartilage ---much like the thick tread on a new tire. This joint is also filled with synovial fluid, which acts like oil, ensuring everything glides without friction.
In osteoarthritis, that smooth cartilage cushion begins to thin and roughen over time. Without its full protective layer, the space between the bones can narrow, leading to friction. This is the fundamental cause of the stiffness and deep ache you might feel, marking the beginning of the "wear and tear" process in osteoarthritis disease progression.
Summary
Understanding the progression of osteoarthritis is crucial for effective management of the condition. While osteoarthritis can advance over years, recognizing its stages and taking proactive steps can significantly slow down its progression. Key lifestyle changes, such as maintaining a healthy weight and engaging in low-impact exercises, play a vital role in preserving joint health and reducing pain.
The BCI Offloader TCO Knee Brace provides additional support, stabilizing the knee joint and enhancing mobility, which can further delay the need for knee replacement surgery. Empower yourself with knowledge and actionable steps to navigate your osteoarthritis journey while maintaining an active and fulfilling life.
The Four Stages of Osteoarthritis Disease Progression
Progression is rarely a rapid decline, but a journey that unfolds over many years. People often ask, "how quickly does osteoarthritis develop?" For most, the early changes are subtle. The smooth cartilage that caps your bones starts to show minor wear, which might cause an occasional ache after a long walk.
As progression continues into the mild stage, this cartilage thins further. Your body may then try to stabilize the joint by creating small, bony growths called bone spurs (osteophytes). These are not sharp "spurs" like the name suggests, but rather the body's clumsy attempt at repair, which can cause noticeable stiffness or pain.
If the condition gets worse, you might reach a moderate stage. In this stage, gaps in the cartilage leave the bone without protection, and the space in the joint gets smaller. Pain can become a daily issue.
In the most advanced, severe stage, that protective cushion is almost completely gone. This point is called "bone-on-bone." Here, there is no cushioning. This can cause ongoing pain, stiffness, and difficulty moving the joint easily. This severe phase is commonly called end stage; if you're wondering what is end stage osteoarthritis, it's when cartilage is nearly gone and joint replacement may be considered.
This may sound scary, but this journey usually takes many years. Most people do not reach the hardest stage. Most importantly, your diagnosis is not your destiny. Knowing what's happening inside your body gives you the power to make a difference.
How to Slow Osteoarthritis Progression: Two Proven Lifestyle Changes
Knowing how osteoarthritis progresses is only half the story; the other half is about what you can do. If you're asking how to stop osteoarthritis from progressing—or more broadly, what can stop arthritis from progressing—the most reliable answers center on managing your weight and choosing the right kinds of movement.
Think about the load your joints carry. Research shows that for every pound of body weight you lose, you take roughly four pounds of pressure off your knees with each step. This simple change means less daily stress, which can directly reduce pain and slow further cartilage wear.
Movement is also crucial, but the type of movement matters. The goal is to strengthen the muscles that support your joints without pounding on them. Walking, swimming, and cycling are great exercises for stiff joints from arthritis. They help increase stability. In contrast, high-impact activities like running or jumping can often make symptoms worse.
What to Do When Your Joint Pain Suddenly Worsens: Managing Flare-Ups
Even if you have good daily habits, you might still have a flare-up of osteoarthritis. This means you can feel more pain, swelling, or stiffness for a short time. These episodes are often triggered by overdoing an activity, like gardening for an extra hour or walking on uneven ground. While frustrating, a flare-up is a common part of managing the condition and doesn't mean your OA is rapidly advancing.
For most mild flare-ups, you can find relief at home. An effective method involves four simple steps:
Rest the Joint: Give it a break from strenuous activity for a day or two.
Apply Ice: Use a cold pack wrapped in a towel for 15-20 minutes to calm inflammation.
Use Gentle Compression: An elastic bandage can provide support and help control swelling.
Elevate It: Prop up your joint to help reduce fluid buildup.
However, it's important to know when to call your doctor. If the pain is bad, doesn’t get better after a few days at home, or comes with a fever or a lot of redness, you should see a doctor.

Can You Reverse the Damage? A Realistic Look at Your Options
Can you reverse osteoarthritis damage? Currently, there's no way to regrow lost cartilage. But that's not the end of the story.
Modern treatments focus on something very achievable: dramatically reducing pain, improving joint function, and slowing progression. The goal is a better quality of life, not turning back the clock on the joint itself.
For most people, this begins with non-surgical treatments. Physical therapy, for example, is a cornerstone of OA care. By making the muscles around the joint stronger, you help support it. This support can absorb shock and lessen the strain on the injured cartilage. This approach can significantly ease pain and make daily activities more comfortable.
When pain becomes severe and an X-ray shows the joint space is gone---the "bone on bone" stage---joint replacement surgery is an excellent option. This common and highly successful procedure replaces the worn-out surfaces with new, artificial ones, effectively relieving pain and helping you return to an active, comfortable life.
Your Action Plan for Living a Full Life with Osteoarthritis
Where a diagnosis of osteoarthritis once felt like a frightening verdict, you can now see it for what it is: a manageable condition. Knowing how to slow down its progress helps you feel less afraid. It gives you a clear way to take charge of your joint health.
Your next steps don't have to be complicated. To start managing your joint health, focus on these lifestyle changes:
Move Your Body Gently Every Day.
Maintain a Healthy Weight to Protect Your Joints.
Partner with Your Doctor to create a plan.
Think of this not as an end to your active life, but as the beginning of a new, more mindful relationship with your body. Each good choice you make helps you in the future. An osteoarthritis diagnosis is just a part of your story, not the whole story.
Q&A
Question: How fast does osteoarthritis progress, and will I inevitably reach the "bone-on-bone" stage?
Short answer: For most people, osteoarthritis progresses slowly over many years---often decades---and many never reach the most severe "bone-on-bone" stage. People often ask, "how quickly does osteoarthritis progress?" or "how quickly does osteoarthritis develop?".
Early changes are subtle (minor cartilage wear and occasional aches), and while symptoms can increase over time, your diagnosis is not your destiny. Understanding what's happening and acting on it---especially with movement and weight management---can meaningfully slow progression.
Question: How can the BCI TCO Knee Brace help slow the progression of osteoarthritis and delay the need for knee replacement?
Short answer: The BCI TCO Knee Brace is designed to provide superior support and stability to the knee joint, which can help alleviate pain and reduce the strain on damaged cartilage. By helping to distribute weight more evenly across the joint and stabilizing the surrounding muscles, this brace can reduce discomfort during movement and promote a more active lifestyle.
Consistent use of the BCI TCO Knee Brace, combined with low-impact exercises and weight management, can play a vital role in slowing osteoarthritis progression and delaying the need for knee replacement.
Question: Which types of exercise help osteoarthritis, and which can make symptoms worse?
Short answer: Choose low-impact activities that strengthen muscles and support the joint without pounding it. Walking, swimming, and cycling are especially helpful for building stability and easing stiffness. High-impact activities like running or jumping can aggravate symptoms for many people. The goal is consistent, joint-friendly movement that keeps you strong and mobile.
Question: How does weight loss reduce joint pain and slow progression?
Short answer: Every pound of body weight you lose takes about four pounds of pressure off your knees with each step. That means less daily stress on cartilage, which can reduce pain and help slow further wear. Even modest, steady weight loss can make a noticeable difference in how your joints feel.
Question: What should I do during an osteoarthritis flare-up, and when should I call my doctor?
Short answer: For most mild flare-ups, use four steps at home: rest the joint briefly, apply ice 15--20 minutes at a time, use gentle compression (like an elastic bandage), and elevate the joint. Flare-ups are common and don't necessarily mean rapid progression. Call your doctor if pain is severe, doesn't improve after a few days of home care, or if you have fever or pronounced redness.
Question: What can stop arthritis from progressing?
Short answer: If you're wondering how to stop osteoarthritis from progressing, the most evidence-based steps are managing body weight, maintaining regular low-impact exercise, and working with your clinician on a personalized plan. These habits support joint stability and can help slow osteoarthritis progression over time.










Comments