Is Osteoarthritis an Autoimmune Disease? Insights
- BCI Health Team

- 2 days ago
- 8 min read
When you hear the word 'arthritis,' what comes to mind? For many people, osteoarthritis causes sore knees and stiff fingers. This condition is often called "wear and tear arthritis."
But then there are autoimmune diseases, where the body's own defense system mistakenly attacks healthy tissue. This has led experts and patients alike to ask a critical question: is osteoarthritis an autoimmune condition?
For years, the answer seemed to be a clear 'no.' Doctors understood OA as purely mechanical damage from a lifetime of use. Recent discoveries are changing things. They show that the immune system plays an important role in how the disease gets worse.
This new understanding of arthritis is more than just a scientific detail. It reframes the entire condition, moving beyond the old story and pointing toward a more hopeful future with better ways to manage your joint health.
Summary
Osteoarthritis is not classified as an autoimmune disease, but low-grade, immune-driven inflammation contributes to its progression after initial mechanical cartilage wear. Rheumatoid arthritis attacks the joint lining strongly from within. In contrast, osteoarthritis has a milder type of inflammation that makes joint damage worse.
This reframes OA as having a significant inflammatory component, opening doors to therapies that target inflammation and protect cartilage. Clear diagnosis distinguishes OA from RA through symptom patterns, autoantibody blood tests, and imaging findings like joint space narrowing. People often ask, "is osteoarthritis an autoimmune disease" or simply "is osteoarthritis autoimmune"; the most accurate answer is no, while acknowledging the immune system’s low-grade involvement.
The Classic Story of Osteoarthritis: What is "Wear and Tear" Arthritis?
For decades, the most common way to understand osteoarthritis (OA) has been as a straightforward "wear and tear" problem. Think of the tread on a car tire that gradually thins out after thousands of miles on the road. This simple, mechanical idea has long been the main explanation for why joints become painful and stiff, particularly as we age.
The Centers for Disease Control and Prevention (CDC) identifies several risk factors associated with osteoarthritis, including joint injuries caused by overuse, such as frequent bending of the knee or consistent pressure on a joint; advancing age; being female, particularly after the age of 50; excess body weight, which places additional stress on the hips and knees; genetics; and race. If you're interested, more information about osteoarthritis can be found. Rheumatoid arthritis, one type of arthritis, can be particularly disabling.
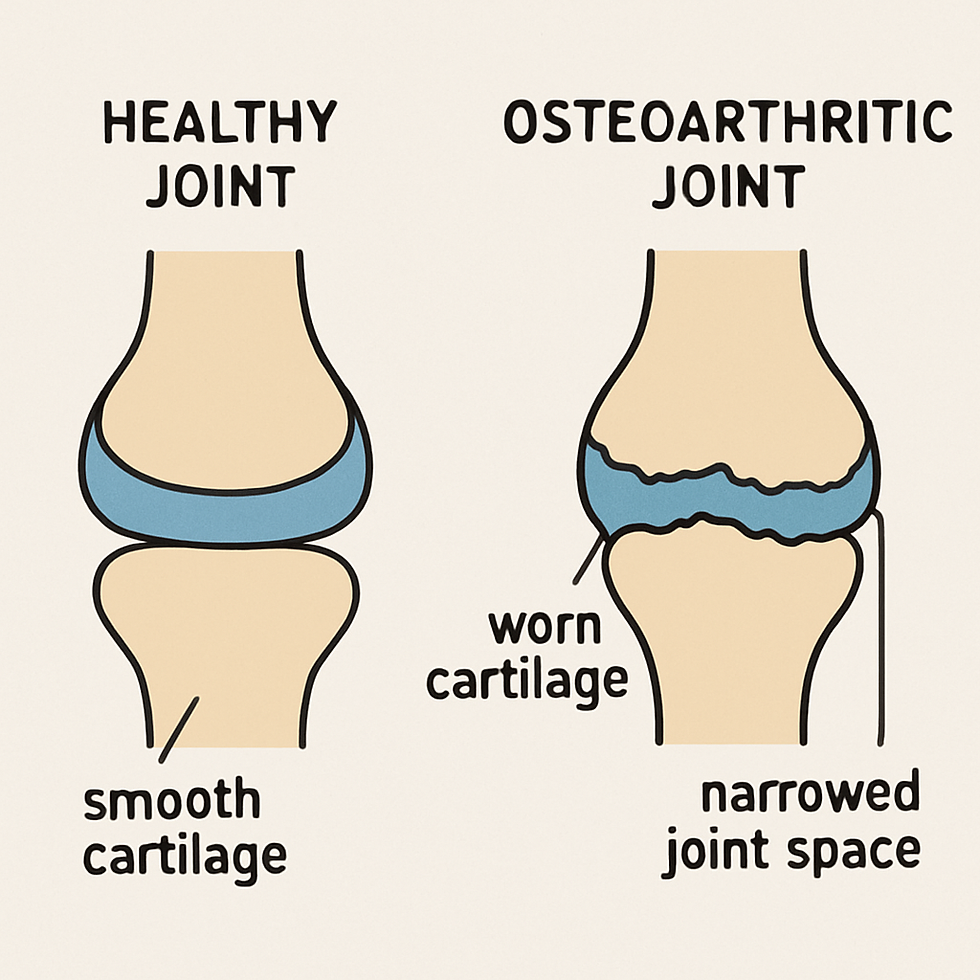
At the center of this story is a remarkable tissue called cartilage. Imagine it as the smooth, slippery cushion that caps the ends of your bones. In a healthy joint, a tough, flexible material helps your bones move smoothly against each other. It also absorbs shock during your daily activities.
In the classic view of OA, years of use, stress, and old injuries cause this cartilage to fray and wear down. As the protective cushion gets thinner, the space between the bones shrinks---a key sign doctors call joint space narrowing. This can make bones rub against each other. This causes pain and a grinding feeling that is often felt in osteoarthritis (OA).
This mechanical explanation makes a lot of sense, and it's a huge part of the puzzle. It explains why OA often appears in hard-working joints like the knees, hips, and hands. But if it were just a mechanical issue, why do some joints get warm or swollen? This question points toward a different kind of joint problem, one driven not by wear, but by the body's own defense system.
Autoimmune Arthritis: When Your Body's Defense System Gets Confused
That feeling of warmth or swelling in a joint hints at a completely different process, one driven by your body's own protectors. In a healthy person, the immune system is a brilliant security force, identifying and attacking invaders like bacteria and viruses. But sometimes, it makes a mistake. In an autoimmune response, this system gets confused and mistakenly targets your own healthy tissues in a case of friendly fire.
The most famous example of this in the joints is rheumatoid arthritis (RA). It is a classic autoimmune disease—one of the most widely recognized autoimmune diseases—and understanding it helps clarify what osteoarthritis is not. In RA, the immune system doesn't primarily attack the cartilage. Instead, its main target is the synovium, the delicate lining that encloses the joint capsule. This lining becomes the primary battleground.
When this wrong attack happens, the synovium gets very inflamed and swells. This causes strong pain, stiffness, and warmth, which are common signs of an RA flare-up. The image shows how the inflamed lining attacks the joint. This damage erodes the healthy cartilage and bone, hurting the joint from the inside.
OA was seen as mechanical "outside-in" damage, while RA was an autoimmune "inside-out" attack. For decades, this separation was simple and absolute.
If that is the complete story, then why are scientists finding signs of the immune system in cases of osteoarthritis?
The Telltale Clue: Why Scientists Started Questioning the OA Story
The search for an answer led scientists to look closer inside the joints of people with osteoarthritis. They expected to find mechanically damaged cartilage and bone, like a frayed rope.
What they found instead was a surprise: the area was full of immune cells. These are the body's first responders, the very same types of cells that rush to a cut or fight off the flu. Their presence in what was supposed to be a simple "wear and tear" condition was a major clue that the story was more complex.
In osteoarthritis (OA), the immune activity is not as intense as in rheumatoid arthritis. It is more like a slow, small fire rather than a big, burning one.
It creates a state of low-grade inflammation. This constant, low-level buzz from the immune system is what can make your OA joint feel warm, puffy, or tender. It explains why the pain isn't always just from movement, but can sometimes feel like a dull, persistent ache even when you're resting.
Crucially, this low-level inflammation isn't just a side effect; it's a participant in the damage. The chemicals from these immune cells can harm the healthy cartilage over time, making it weaker.
This starts a bad cycle. The first damage to the cartilage brings in immune cells. Their response causes even more cartilage to break down. This discovery changed everything, showing that OA isn't just a mechanical problem---it's a biological one, too.
The Real Answer: Think "Dimmer Switch," Not "On/Off"
So where does this leave us?
The best way to see the difference is to think of the immune system like a dimmer switch. It's not just on or off. In a classic autoimmune disease like rheumatoid arthritis, the switch is flipped all the way on, signaling a full-blown attack on your joints. With osteoarthritis, that dimmer switch is just turned up slightly, creating a constant, low-level hum of inflammation.
This is why, to be precise, doctors do not classify osteoarthritis as an autoimmune disease. The crucial difference lies in what starts the problem.
In RA, the immune system is the primary attacker, kicking down the door to a healthy joint. In OA, the door was already hurt from pressure. The immune system's response makes the problem worse as time goes on.
Because of this inflammatory component, many experts now place osteoarthritis in a broader category of inflammatory arthritis. Your immune system doesn't cause OA, but it becomes an active participant that worsens it. An old injury or years of use can start the problem. The ongoing swelling is what causes more damage and pain.
Ultimately, this reclassification is more than just a change in terminology. Viewing osteoarthritis as a disease with a strong inflammatory part—something some researchers call primary inflammatory osteoarthritis—changes the whole discussion. It helps us go beyond just treating symptoms. We can focus on one of the main causes of the disease.
Why This New Understanding Is a Game-Changer for You
Thinking of osteoarthritis as simple mechanical wear can feel discouraging, suggesting a future of inevitable decline. But seeing it as a condition with an inflammatory trigger changes everything. This change means that researchers are not only searching for better painkillers. They are also looking for new treatments for OA that can reduce the inflammation in the joint.
It opens the door to therapies that could fundamentally alter the course of the disease.
These new treatments have a great promise: they may help slow down the damage to the joints, not just hide the pain. Imagine a treatment that not only eases pain but also helps protect your cartilage from damage caused by long-term joint swelling. This new approach is about managing osteoarthritis better over time. It goes beyond just easing symptoms and aims to really protect the joints.
This knowledge empowers you in conversations with your doctor. You can now ask about strategies that address the inflammatory component of your pain, not just the mechanical aspect. It's important to understand that your OA has a different cause and immune response than a typical autoimmune disease.
It ensures you get the right diagnosis, which is the most important first step toward the right treatment plan.
How Doctors Pinpoint the Right Diagnosis: OA vs. RA
Given that both conditions cause painful joints, you might wonder how your doctor can confidently tell them apart. To tell the difference between classic rheumatoid arthritis and osteoarthritis, you need a thorough examination that goes beyond just looking at your symptoms. This process combines your story with powerful diagnostic tools to get a complete picture.
By piecing together these different clues, your doctor can determine the specific cause of your joint pain. This three-part investigation almost always includes:
Symptom Pattern: Rheumatoid arthritis often affects joints symmetrically---for example, in both wrists or both knees at the same time. Osteoarthritis, on the other hand, can be one-sided and is more common in large, weight-bearing joints.
Blood Tests: This is a crucial step. Specific blood tests for autoimmune arthritis look for "mistaken identity" flags called autoantibodies (like RF and anti-CCP). These proteins show that the immune system is attacking. They are signs of rheumatoid arthritis (RA) but are not found in osteoarthritis.
Imaging: An X-ray provides a direct look at the joint's physical condition. In OA, the key finding is a narrowing of the space between the bones, which shows that the cartilage cushion has worn down.
Your doctor can make a correct diagnosis by looking at your symptoms along with blood test results and X-rays. This crucial step ensures you receive a treatment plan tailored specifically to the true cause of your pain.
Your Next Steps: Turning This Knowledge into Action
You once may have thought of osteoarthritis as simple wear and tear---a part wearing out.
Now you can understand better: your immune system is more active, causing a steady level of inflammation. This can lead to pain and damage. This shift from a mechanical problem to a biological one is a powerful change in perspective.
This new view on managing osteoarthritis doesn't mean it's an autoimmune disease. Instead, it simply puts inflammation on the map as a key target.
Understanding this difference is the first step to having better talks about your health and discovering new information about osteoarthritis.
Your knowledge is now your power. When talking to your doctor about arthritis, you can move the conversation forward. At your next appointment, ask: "Besides managing pain, what can we do about the inflammation in my osteoarthritis?"
This single question transforms you into an active partner in your care.
Frequently Asked Questions (FAQs)
What are the common symptoms of osteoarthritis?
The most common osteoarthritis symptoms include joint pain, stiffness, swelling, and a decreased range of motion. Patients may also experience a grating sensation during movement and bone spurs. It's important to recognize these symptoms early for better management.
Is osteoarthritis an autoimmune disease?
No, osteoarthritis is not classified as an autoimmune disease. It is mostly caused by wear and tear on the joints. However, recent studies show that inflammation may also contribute to its worsening.
How can I improve my joint health with osteoarthritis?
Improving joint health with osteoarthritis often involves a combination of physical activity, weight management, and possibly the use of supportive devices like hinged knee braces. These braces can provide stability to the knee and help reduce pain during movement.
Are there any innovative treatments for osteoarthritis?
Yes, there are several innovative treatments for osteoarthritis being researched and developed, including therapies aimed at reducing inflammation and protecting joint cartilage. It's advisable to discuss these options with your healthcare provider.
What is the role of a hinged knee brace in managing osteoarthritis?
A hinged knee brace can be particularly beneficial for individuals with osteoarthritis of the knee. It provides support, helps stabilize the joint, and may alleviate pain, allowing for improved mobility and functionality. Incorporating a hinged knee brace into your treatment plan can be a proactive step in managing symptoms.










Comments